Introduction
In healthcare, Diagnosis-Related Groups (DRGs) have been a fundamental tool since their origin in 1980. However, despite their effectiveness in classifying patients and optimizing resources, their large-scale adoption has faced obstacles. Now, in the age of artificial intelligence, DRGs are making a comeback. In this article, we talk about their advantages and challenges, as well as their role in the transformation of healthcare towards value-based healthcare models.
What are DRGs?
Have you ever come across ideas that were ahead of their time? I would venture to say that this is what happened with the adoption of Diagnosis-Related Groups or DRGs. But today, for different reasons, they are re-emerging.
Diagnosis-Related Groups are a patient classification system that allows a hospital to organize its healthcare activities by relating the different types of patients treated to the cost of their care.
Suppose someone needs hip replacement surgery. The cost of treatment of that patient, both for the healthcare entity providing care and for the insurer or funder that will then reimburse the hospital, can be determined in a number of ways.
A classic way to determine the cost of treatment is to reimburse one by one the amounts due for each of the practices performed (for example, fees, diagnostic imaging, laboratory tests, etc.), the consumables required by the patient (disposables, medication, prostheses, etc.), and the use of the different areas of the hospital (operating room hours, hospital beds, etc.). It is a logical and widely used form of “Fee For Service.” But, as you can imagine, nothing tells us if the practices performed were adequate. This method involves the risk of overuse of procedures, as there is little incentive for efficiency in the use of resources linked to the medical results achieved in the patient.
Another method to determine the cost is to put together specific modules or packages that are priced based on historical data of patients’ use of practices, services, products and times, adjusted for factors such as each patient’s risk profile and specific characteristics.
These modules or packages make it possible to determine with greater certainty the average cost of care, as well as its maximums and minimums derived from the specifics of each case, since medicine is not an exact science, and each patient (and disease) has its variations (episodes). Ultimately, the care provider is reimbursed the cost of a given module.
One advantage of module-based payment models is that they make it possible to standardize healthcare practices, thereby making them comparable between hospitals as well as with norms or standards of care. This module-based method, which allows for comparison between patients and institutions and encourages efficiency, is known as the International DRG Methodology.
Since their adoption, DRGs have proven to be a fundamental tool for cost control in healthcare and for improving the quality of care. These are some of their key advantages:
- Increased efficiency in hospital bed management.
- Increased transparency and reduced friction in payer-provider relationships.
- More effective use of healthcare resources.
- Reduction of administrative costs that do not add value for payers, hospitals or patients.
Despite their seemingly simple logic and time-tested effectiveness, the question arises as to why DRGs haven’t been implemented on a large scale worldwide.
Well, there are nuances…
DRGs offer an efficient way to classify patients according to patterns of care (clinical similarity) and similar costs (iso-consumption). This allows for more accurate resource allocation, benchmarking of quality of care, and more accurate prediction of costs and reimbursement. However, its implementation may face challenges in terms of data standardization, information requirements necessary for its use, and resistance to change from health systems or their decision-makers.
The implementation of the algorithms used in Diagnosis-Related Groups (DRGs), along with the change management required during the introduction of a new payment method, is not a merely technical process. The politics surrounding the introduction of the system and the expected change in resources will generate both supporters and opponents. Therefore, strong technical capacity is required from buyers, suppliers and health ministries or other relevant regulatory agencies to manage the DRG system, as well as the necessary change management involved.
Among the components and technical processes required, we’d like to highlight the following:
- DRG algorithms: The development of a national and public classification algorithm is the most technically complex task. For this reason, most countries start with an imported DRG grouping algorithm or use an existing one as reference, adapting it to the country’s context. International experience shows that adaptations to the health information management system, the contracting and payment modalities, and the imported DRG algorithm require several years.
- Effective hospital information system: The quality of basic data is fundamental to the implementation of a DRG system. However, a DRG system can, over time, encourage and continually improve data collection for this and other health policy purposes. There is a need for electronic medical records based on standardized coding systems, as well as cost accounting systems by episode and by DRG.
In conclusion, deficiencies in data collection or data quality should not be an obstacle for a country or an organization to implement a DRG model, as these are tools that contribute to the objectives of universal health coverage. The incentives established by the system must be carefully considered to ensure that comprehensive care is centered on people, and not solely on economic considerations.
The Current Resurgence
In the era of AI and digital health, DRGs are experiencing a resurgence due to their ability to integrate with advanced technologies and leverage large volumes of medical data. Standardization and clustering of case reports, clinical and economic benchmarking, as well as decision support systems and predictive analytics, are enhancing the role of DRGs in the transformation of medical care.

To take full advantage of DRGs today, it is crucial to ensure standardization and quality of medical data, as well as interoperability between different health systems and digital platforms. In addition, collaboration between HealthTech companies, healthcare professionals and regulators is needed to ensure data privacy and security.
AI, data analytics and digitalization of electronic medical records are key enabling technologies that are driving the resurgence of DRGs. These technologies enable more accurate patient classification, more efficient resource optimization and more informed clinical decision making.
Why Globant and Avedian?
At Globant Healthcare & Lifesciences AI Reinvention, we are working with Avedian to offer advanced digital health solutions that integrate DRGs with AI technologies and data analytics. Our services include the implementation of end-to-end systems using proprietary DRG algorithms customized to the reality of each country and each organization, the optimization of hospital workflows and the improvement of the quality of medical care through artificial intelligence and the latest advances in technology.
With more than 40 implementations in the region, we have the experience, equipment and scale available to transform how healthcare organizations today face challenges such as medical process auditing, the rising costs of innovative pharmaceutical products and the transformation to value-based payment models.
To each project, we bring Globant’s capabilities as one of the most renowned software and technology companies in the world and the expert knowledge on healthcare systems and their challenges, urgencies and needs that Avedian provides.
Proprietary DRG algorithms, both for hospital and population-based cases, are available from the beginning of each project, which is one of the reasons why our implementation times for DRG projects, whether in analytics or as a paid model, are around two to three months in hospitals and six to eight months in health insurance.
Credentials and Case Studies
Case 1: Keralty Group – Colsanitas private hospital network (Colombia)
Colsanitas, a leading organization in Colombia dedicated to offering comprehensive health services through its network of health promoting entities and hospitals, as well as its insurance division, is part of the Keralty Group, with presence in multiple countries.
Colsanitas has implemented the Diagnosis Related Groups (DRG) methodology to transform its hospital network management model, marking an important milestone towards the optimization of healthcare.
This approach has allowed for better resource planning, more efficient allocation of funds and more personalized care for each patient, in line with the patient-centered care paradigm. The results have been remarkable:
- Significant increase in bed management efficiency, achieving a 35% reduction in waste in hospital admissions.
- Significant increase in the safety of hospitalized patients, with a 27% decrease in avoidable complications.
- Optimization of hospital processes, reflected in a 5% reduction in avoidable readmissions.
Case 2: APROSS (Administración Provincial del Seguro de Salud de Córdoba, Argentina)
APROSS is Córdoba’s provincial health insurance administration, an entity that provides health coverage and insurance to active and passive agents of the three branches of the provincial government and the affiliated municipalities and neighborhoods. It may also provide coverage to other individuals or groups through voluntary affiliation.
It has a community of more than 630,000 members and is one of the 5 largest insurance companies in Argentina. It has a network of nearly 350 single and multipurpose hospitals, its own 400-bed hospital and 15,000 other providers. It also offers discounts in 1,600 participating pharmacies.
In APROSS, the DRG methodology was used to restructure the entire provider payment model, previously based on fixed budgets, towards a value-based healthcare model. This led to the following results:
- 32% cost optimization by reducing waste in avoidable hospitalization days.
- 40% decrease in the network’s average length of stay (out of a total of 90,000 hospitalizations per year).
Additionally, the DRGs were used for integration and advanced data analysis, which allowed stratification according to risk levels of the population of members and better planning of prevention, disease and case management strategies.
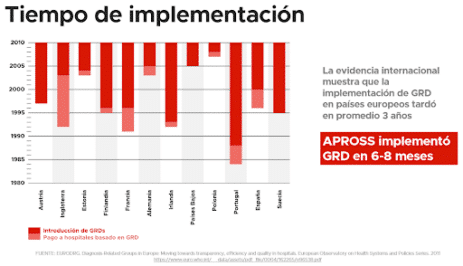
According to international evidence, it took an average of three years to implement reforms similar to APROSS. But thanks to proprietary DRG algorithms and specific technology, we were able to reduce these implementation times to 6-8 months.
What’s our approach?
How Avedian and Globant facilitate DRG implementation and enhance its role as an analytics tool
At Globant Healthcare & Life Sciences AI Reinvention, together with Avedian, we offer advanced digital health solutions that integrate our proprietary DRG algorithms with AI technologies and data analytics. Our services include implementing customized DRG systems, optimizing hospital workflows, and improving the quality of care through AI and the latest technological advances.
With extensive experience in the region, we have led numerous successful implementations in record time that have transformed the way healthcare organizations address challenges such as medical process auditing, cost management and the transition to value-based payment models.
In short, DRGs are experiencing a renaissance in the era of AI, enhancing their role as a management and analytical tool in healthcare. With the support of companies like Avedian and Globant, we are redefining the way healthcare data is managed, driving a significant transformation in healthcare delivery toward more efficient and value-centric models for patients.
Authors:
Dr. Guillermo Tabares Martinez – Avedian CEO & Co-Founder
Dr. Lucas Najún Dubos – Globant Healthcare & Life Sciences Partner
- Blog Gestión Sanitaria
- The Evolution of Diagnosis-Related Groups (DRGs): From Its Beginnings in Case-Mix and Resource Use Theory, to Its Implementation for Payment and Now for Its Current Utilization for Quality Within and Outside the Hospital. Quality Management in Health Care. 2009
- Transition to DRG Payments for Health: Lessons from Case Studies. International Development in Focus. Washington, D.C: World Bank; 2019.
- Diagnosis-Related Groups in Europe: Moving towards transparency, efficiency and quality in hospitals. European Observatory on Health Systems and Policies Series. World Health Organization. 2011
- Assessing health provider payment systems. A practical guide for countries working towards universal health coverage. Washington (DC): Joint Learning Network for Universal Health Coverage; 2015
- Key aspects related to implementation of risk stratification in health care systems. The ASSEHS study. BMC Health Services Research. 2017
- The long-run effects of diagnosis related group payment on hospital lengths of stay in a publicly funded health care system: Evidence from 15 years of micro data. Health Economics. 2022
- Health Technology, Quality, Law, and Ethics.The New Public Health (Third Edition). 2014
- Using diagnosis-related groups for studying variations in hospital admissions. Health Care Financ Review. 1988
- The effects of diagnosis-related groups payment on hospital healthcare in China: a systematic review. BMC Health Services Research. 2020
- DIAGNOSIS-RELATED GROUPS (DRG): A Question & Answer guide on case-based classification and payment systems. World Health Organization. 2020
- Challenges of implementing diagnostic‐related groups and healthcare promotion in Iran: A strategic applied research. Health Science Report. 2023
- https://youtu.be/EwB5rmdh7H0
- https://aws.amazon.com/es/solutions/case-studies/apross-case-study/
- EURODRG. Diagnosis-Related Groups in Europe: Moving towards transparency, efficiency and quality in hospitals. European Observatory on Health Systems and Policies Series. 2011




